
Get the full story of the microbiome
- Importance of Microbial Diversity
- Dysbiosis and Recurrent C. difficile Infection
- Historic Microbiome Restoration Approaches
- Patient and Healthcare Burdens
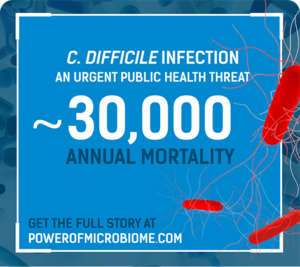
C. difficile infection (CDI) is one of the most common
healthcare-associated infections in US hospitals, affecting
approximately half a million people annually.1,2

Patient Burden

Recurrence is a vicious cycle
- Up to 35% of patients experience recurrence1,3,a
- Up to 65% of patients experience subsequent recurrences4,5

Physical and psychological suffering continues
From a 2017 study that surveyed patients with CDI or recurrent CDI (rCDI), a majority of 350 patients who have experienced CDI or rCDI report physical and psychological symptoms6
- 41% of patients believed they would never get rid of post-CDI symptoms6

CDI can lead to significant complications including sepsis, colectomy, and mortality
Sepsis
- 27% of patients (aged 18 to 64 years) with one recurrence experienced
sepsis during 12-month follow-up7,b
Colectomy
- 7% of patients with one recurrence had a colectomy during 12-month
follow-up7,b
Mortality
- 6% of patients with index CDI within 30 days of diagnosis1
- 25% of Medicare patients with rCDI at 12 months8
- 52.5% of Medicare patients with rCDI who developed sepsis at 12
months7,b
Other severe complications in patients include heart failure (43%),9,c anxiety (14%),10,d and depression (15%).10,d
aWithin 8 weeks after initial CDI diagnosis.
bLongitudinal, retrospective study of the US PharMetrics Plus™ database reported on complications of CDI recurrence over 1 year (N=46,571) from a single referral center.
cRetrospective study of a Medicare claims analysis of patients with CDI (N=268,762).
d12-month follow-up of retrospective cohort study at first recurrence (N=38,163).

Healthcare Burden

Hospitalizations
- Up to 84% of all patients with rCDI were hospitalized within a year in a single center study11
- Up to 85% of all patients with rCDI were readmitted within a year in a single center study12
Length of stay
- Hospitalizations averaged 18 days for patients with rCDI in a single center study of Medicare patients >65 years of age9

Costs
- $131K to $207K in total direct costs per patient with rCDI within a year in a study of state institutional databases13
- A -$3K to -$29K gap existed in reimbursement per patient with rCDI in a study of state institutional databases14
According to the CDC, CDI is classified as an immediate public health threat requiring aggressive, urgent action15
THE BURDEN OF CDI MAY INCREASE
WHEN THE INFECTION RECURS
Can the power of the microbiome be
unlocked to break the cycle of rCDI?
Share this with colleagues!
Ferring is committed to exploring the potential of a microbiome-based therapeutic that is studied in a comprehensive population reflective of routine clinical practice for the treatment of recurrent C. difficile infection.
References
- Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825-834.
- Guh AY, Mu Y, Winston LG, et al. Trends in U.S. burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2021;382(14):1320-1330.
- Cornely OA, Miller MA, Louie TJ, Crook DW, Gorbach SL. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis. 2012;55(suppl 2):s154-s161.
- Kelly CP. Can we identify patients at high risk of recurrent Clostridium difficile infection? Clin Microbiol Infect. 2012;18(suppl 6):21-27.
- Smits WK, Lyras D, Lacy DB, Wilcox MH, Kuijper EJ. Clostridium difficile infection. Nat Rev Dis Primers. 2016;2:16020.
- Lurienne L, Bandinelli PA, Galvain T, Coursel CA, Oneto C, Feuerstadt P. Perception of quality of life in people experiencing or having experienced a Clostridioides difficile infection: a US population survey. J Patient Rep Outcomes. 2020;4(1):14.
- Feuerstadt P, Boules M, Stong L, et al. Clinical complications in patients with primary and recurrent Clostridioides difficile infection: a real-world data analysis. SAGE Open Med. 2021;14(9):2050312120986733.
- Feuerstadt P, Nelson WW, Drozd EM, et al. Mortality, health care use, and costs of Clostridioides difficile infections in older adults. J Am Med Dir Assoc. 2022;S1525-8610(22)00153-0. doi: 10.1016/ j.jamda.2022.01.075.
- Nelson WW, Scott TA, Boules M, et al. Health care resource utilization and costs of recurrent Clostridioides difficile infection in the elderly: a real-world claims analysis. J Manag Care Spec Pharm. 2021;27(7):828-838.
- Scott TA, Unni S, Boules M, et al. Clinical burden of recurrent Clostridioides difficile infection in the Medicare population. Presented at: 2020 Digestive Disease Week; May 2-5, 2020; Chicago, IL.
- Rodrigues R, Barber GE, Ananthakrishnan AN. A comprehensive study of costs associated with recurrent Clostridium difficile infection. Infect Control Hosp Epidemiol. 2017;38(2):196-202.
- Olsen MA, Yan Y, Reske KA, Zilberberg M, Dubberke ER. Impact of Clostridium difficile recurrence on hospital readmissions. Am J Infect Control. 2015;43(4):318-322.
- Feuerstadt P, Stong L, Dahdal DN, Sacks N, Lang K, Nelson WW. Healthcare resource utilization and direct medical costs associated with index and recurrent Clostridioides difficile infection: a real-world data analysis. J Med Econ. 2020;23(6):603-609.
- Zilberberg MD, Nathanson BH, Marcella S, JJ Shorr. Hospital readmission with Clostridium difficile infection as a secondary diagnosis is associated with worsened outcomes and greater revenue loss relative to principal diagnosis: A retrospective cohort study. Medicine. 2018;97(36):312212.
- Centers for Disease Control and Prevention website. 2021 Antibiotic Resistance Threats Report: Clostridioides Difficile. https://www.cdc.gov/drugresistance/pdf/threats-report/clostridioides-difficile-508.pdf. Accessed March 12, 2022.
