C. diff: The inside story
Let’s start with the basics. Gain a better understanding of C. diff and what to expect during this illness. What you learn may help when making health-related choices with your doctor.
What is a C. difficile infection?
C. diff is short for the name of the germ that causes the infection: Clostridioides difficile.
C. diff can affect anyone. The risks are greater for people who1:
- Are taking, or have recently taken, antibiotics
- Have spent some time in a hospital or in a long-term care facility,
such as a nursing home - Have a weakened immune system
- Are 65 years of age or older
When C. diff germs take hold and multiply in the gut (intestines), they can wreak havoc.
This center of gut health is called the microbiome. When it gets out of balance your
health is at risk, and infections like C. diff can result.2-4
The most common symptoms—watery diarrhea, nausea, stomach pain or cramps—can last for days.
If not treated right away, C. diff can lead to serious medical problems for the person who has it. A severe
C. diff infection can be fatal for certain people.1,5
Many people may not realize that getting a relapse of the infection is highly possible. This is called recurrent C. diff.6-9
Learn about treatment for recurrent C. diff infection.
Did you know? C. diff is very contagious and can become a serious health threat
to others in the home and the community.1,10,11
Download our C. diff information brochure here
Understanding C. diff infection
How can you get C. diff?
Since it is very contagious, it’s important to be aware of ways that C. diff can spread1,10:

Direct contact
Someone who has C. diff can
spread the germs to people
they touch.

By indirect contact
If you come into contact
with a caregiver of someone with
C. diff, they may have picked up the
germs, and could pass them on.

Contaminated surfaces
If a person with C. diff does not wash
their hands after using the bathroom,
the germs can spread to others who
touch the things they touched.
Did you know? C. diff germs could be in your body and not cause symptoms. Even though you don’t feel sick, you can still spread the germs to others who may develop a serious infection.
C. diff and the microbiome connection
 Think of the gut microbiome as our own collection of microscopic life forms—microbes that play a role in how our bodies work. The gut microbiome (in the stomach and intestines) is home to trillions of microbes, both good and bad, that can affect many aspects of our health.2-4
Think of the gut microbiome as our own collection of microscopic life forms—microbes that play a role in how our bodies work. The gut microbiome (in the stomach and intestines) is home to trillions of microbes, both good and bad, that can affect many aspects of our health.2-4
Health in the balance
A balanced microbiome helps your body in many ways.3,4,12
- It aids with the way the body breaks down and absorbs nutrients from food
- It works with the immune system to protect you from infection
- New research also links the microbiome to blood sugar control, brain function, heart health, and overall gut health
Did you know? An imbalance in the microbiome may give harmful bacteria like C. diff the chance to take hold and grow in the gut. This can lead to a C. diff infection. Microbiome imbalance also plays a role in medical problems such as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD).5,12
Learn about treatment for recurrent C. diff infection.
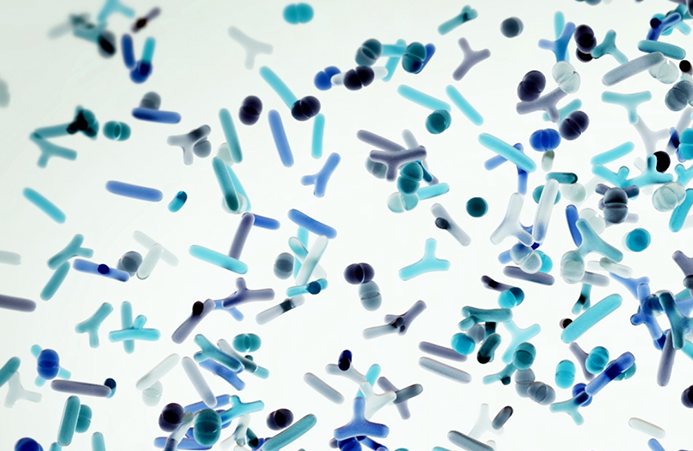
This is a healthy microbiome. It has a diverse mix of bacteria, including generally helpful species called Bacteroides.
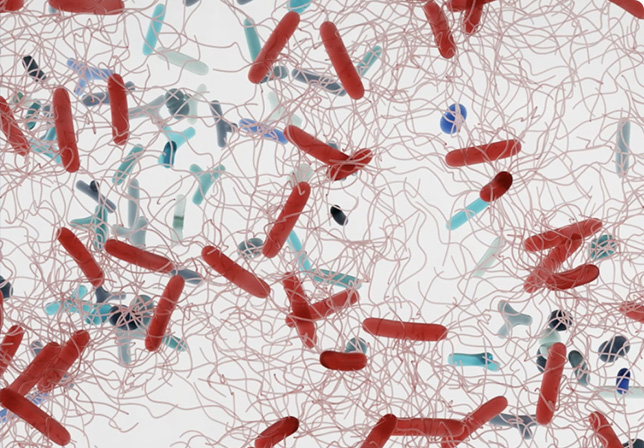
This is a microbiome that’s out of balance. C. diff has grown, and could make you very sick.
Know the symptoms
C. diff infection can take people by surprise. They may think “It’s just a stomach bug!” or some other familiar digestive problem. It’s important to recognize the symptoms and know when to go to the doctor for help.
Mild Symptoms1,10
- Watery diarrhea 3 or more times a day for more than 1 day
- Mild abdominal cramping and tenderness
Moderate to Severe Symptoms1,10
- Watery diarrhea, as often as 10 to 15 times a day
- Abdominal cramping and pain, which may be severe
- Rapid heart rate
- Dehydration
- Fever
- Nausea
- Increased white blood cell count
- Kidney failure
- Blood or pus in the stool
If any of these symptoms last more than 2 days—or quickly get worse—it is recommended that you talk to your doctor.
When to see a doctor10
Don’t be afraid to seek medical help if your symptoms last for more than 2 days. Let your doctor know if you have:
- 3 or more watery stools a day
- A new fever
- Severe abdominal pain or cramping
- Blood in your stool

How to talk with your doctor
Sometimes, people may not know how to tell their doctor about the symptoms they are experiencing. They may be embarrassed to talk about diarrhea or feel it’s just “too much information.” To help start the conversation with the doctor, use the C. diff Checklist.

Tests to confirm a C. diff infection
Most often, the doctor will ask for a sample of your stool (poop). Different lab tests may be done to check the sample for C. diff bacteria.10
For severe C. diff cases, the doctor may also ask for other tests to check the inside of the colon (large intestine). Imaging tests are sometimes done to help reveal other possible problems related to C. diff. For example, to check for any damage to the lining of your colon, special x-ray equipment is used. An x-ray of the abdomen or a computerized tomography (CT) scan are examples of imaging tests the doctor may order.13
How to keep C. diff from spreading
In hospitals and other healthcare facilities—and in patients’ homes—strict
routines for cleanliness need to be in place13,14:
- Hand hygiene. Wash hands with soap and warm water before and after using the bathroom,
and before and after eating - Control contact. People with C. diff need to be isolated in a private room, with a bathroom only
they will use - Use protective gear. Disposable gloves or gowns may be required when near visitors in the hospital
- Disinfect and clean thoroughly. Use products that contain chlorine bleach to kill bacteria. Ordinary alcohol-based cleaners or sanitizers do not kill C. diff.
C. diff information sign-up form
Get access to tools and resources to help you—or someone you care for—cope with this serious and
debilitating condition.

Understanding current C. diff treatment options
Antibiotics and C. diff
Antibiotics are the go-to treatment for a C. diff infection and can be effective.14,15
- For a first-time infection, doctors may prescribe 10-day treatment with an antibiotic to treat C. diff 14,15
- For a recurrent C. diff infection, antibiotic treatment may last for several weeks. The doctor also may slowly decrease or pulse how often the dose is given14,15
Something else to know about antibiotics
Antibiotics kill or stop the growth of the disease-causing C. diff bacteria. But antibiotics further kill some of the good bacteria, like Bacteroides. This disrupts the delicate balance of the microbiome—making it possible for C. diff to take hold.14,17
A cycle of recurring infection
Using antibiotics for extended periods of time, or using more than one antibiotic for treating an illness, may also lead to a cycle of recurring C. diff infections.8,9,19
Fecal Microbiota Transplantation (FMT)
FMT, which can be rectally administered, adds a diverse mix of bacteria into your gut microbiome—helping it get back in balance. FMT may be a good option to consider for people who have had C. diff multiple times, after antibiotic treatment.12,14-16
More about FMT
- With FMT, first a healthy donor provides stool, which is used to make a solution to be used in the treatment
- This solution may be placed into the colon of the person with C. diff during a colonoscopy or upper endoscopy, or with a simple enema (through the rectum) done by the doctor
- FMT has been shown to have a cure rate in the range of 68% to 83% for C. diff18
Talk to your doctor about the C. diff treatment option that may be right for you.
Learn about treatment for recurrent C. diff infection.
What about probiotics?
Probiotics are not recommended for use to prevent or treat a C. diff infection. They can be taken safely when your gut is in a healthy state, and they are designed to help maintain a healthy gut microbiome.20,21
In fact, after antibiotic treatment, probiotics may actually stop the process by which the microbiome develops a more normal balance of bacteria.22
Before taking any supplements, it is important to talk to your doctor.

Not again?! C. diff can come back
Just when it seems C. diff is done and gone, it comes roaring back. Even after treatment, some people experience repeat infections—this is called recurrent C. diff. The symptoms go away, but then return.6-8
Learn about treatment for recurrent C. diff infection.
C. diff by the numbers
Around
HALF A
MILLION
infections are
caused by C. diff
every year6,11
Up to
3 IN 10
PEOPLE
who get a C. diff infection
will get it again7
After 1st recurrence, up to
6 IN 10
PEOPLE
will get another
C. diff infection8,9
About
8 IN 10
PEOPLE
with recurrent C. diff
were hospitalized in
12 months, and at
least 3 separate
times23,24
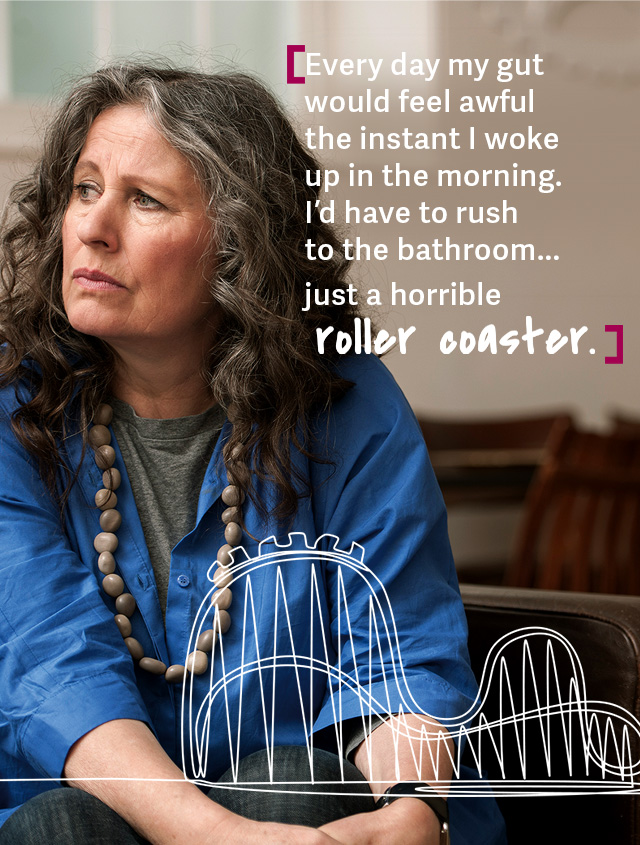
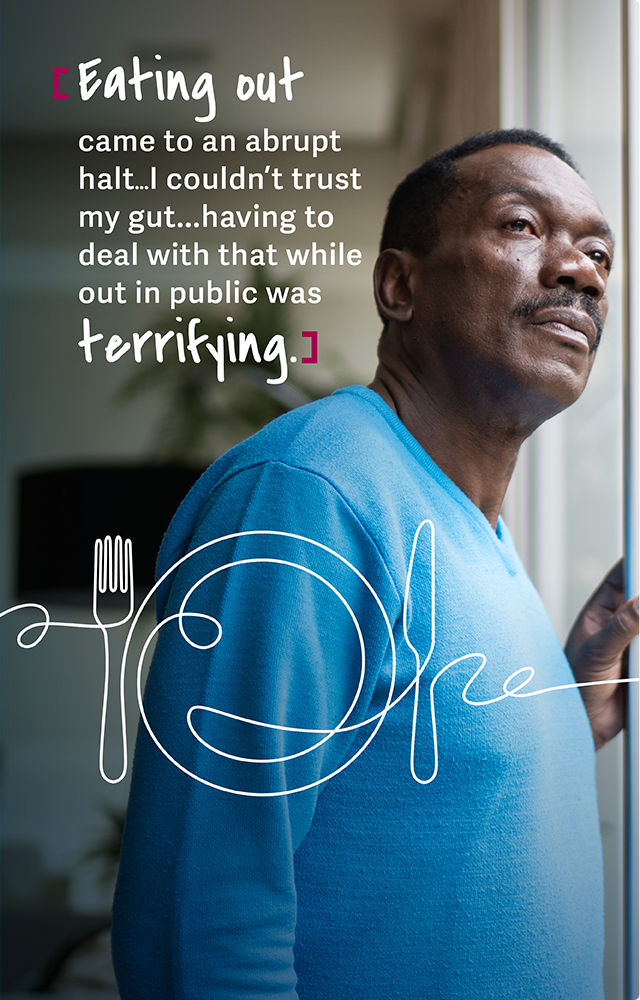
Recurrent C. diff can affect your mental health, too
The effects of recurrent C. diff sometimes go beyond physical pain. It can trigger depression and other mental health concerns, too. People have described how C. diff has taken a toll on their lives25:
- Many people struggle with other physical effects of C. diff—loss of energy, appetite, or sleep
- A C. diff infection, with the constant diarrhea and other symptoms, may strain a person’s relationships with family, friends, or significant others
- C. diff has forced people to limit or give up travel, outdoor activities or events, and even enjoying different types of food
If you are feeling this way, talk with your doctor or a mental health professional for guidance and support.
Here is a helpful resource from the National Institute of Mental Health:
Information and inspiration
Click on the videos below to see stories of strength from patients and caregivers. Learn how you can get involved in an online panel. And understand how food and nutrition play a part in recovery from C. diff.
Patient stories
With almost half a million cases of C. diff infections every year,6,11 why don’t we hear more about it? See hopeful stories of people who have struggled with and overcome C. diff.

Help and inspire others with C. diff. Be part of an online research panel.
Be compensated for sharing your experience as a patient or caregiver. Take part in a variety of
anonymous, online surveys and exercises that won’t take much of your time, and may help others.
Food: friend or foe?
People experiencing C. diff lose their appetite, or fear that food will trigger diarrhea. However, good nutrition is vital to recovery. The body needs to regain strength and rebuild gut health. Make sure to ask your doctor about what you can eat during and after C. diff.




According to the Mayo Clinic, a supportive diet may include26:
- Plenty of fluids to prevent dehydration—choose drinks that contain water, salt, and sugar. For example, watered-down
juices, soft drinks, or broths - Starchy foods, such as potatoes, noodles, rice, or wheat
- Simple foods, such as saltine crackers, bananas, soup, and boiled vegetables
Talk to your doctor or a nutritionist for guidance on C. diff-friendly food choices.
And be sure to sign up to get more useful information!
Fact or fiction? C. diff and food
Experts continue to study how nutrition—and boosting the microbiome—can help with recovery after C. diff. There is so
much to learn. Do you know which of these is fact or fiction?
Milk and milk products are helpful after a C. diff infection
- FICTION: After a C. diff infection, some people may have symptoms of irritable bowel syndrome (IBS). As a result, they can become lactose intolerant—unable to take in milk and other dairy foods. Nutrition experts advise avoiding these foods for at least 2 to 4 weeks.27
Certain diets may help improve or decrease the chances of getting a C. diff infection
- FACT: Several studies have shown that a Western diet (high protein, high fat, low fiber) or a gluten-free diet may reduce the variety of microbes in the microbiome, while a vegan, or plant-based, diet may build diversity in the microbiome, which may help protect against C. diff infection.27
Fiber-rich foods (beans, grains, fruits, and vegetables) or supplements can help with recovery after C. diff
- FACT: Fiber-rich foods have been shown to help with some medical conditions like IBS, constipation, and with some symptoms that come after a C. diff infection. For example, supplements with a plant-based fiber called psyllium help absorb liquid and bulk up the stool for C. diff patients.27
Coffee or other drinks with caffeine are okay to take while recovering from C. diff
- FICTION: Avoid coffee and other caffeinated drinks, at least for a short time, after a C. diff infection because they may cause digestive problems.27
Stay away from greasy foods or spicy foods while recovering from C. diff
- FACT: Avoid greasy or spicy foods while recovering from C. diff as they may also cause digestive problems.27
Talk to your doctor or a nutritionist for guidance on C. diff-friendly food choices.
Recipes for maintaining gut health

Miso Roasted Rainbow Carrots

Blueberry Mango Zinger Smoothie

Miso Roasted Rainbow Carrots
This carrot dish is elegant, colorful, nutritious, delicious, and easy to make. Provides a wonderful side dish to a healthy meal. Carrots are mild, low in fiber, and easy to digest. Cooking them until soft makes them even easier to digest. Consider this recipe gut-friendly!
Ingredients
Yogurt Sauce
- ½ cup plain Greek yogurt
- 1 tablespoon white miso paste
- 1 teaspoon honey or agave
- ½ teaspoon reduced sodium soy sauce (tamari if gluten free)
- 2 teaspoons rice vinegar
Miso Roasted Carrots
- 2 bunches rainbow carrots washed, peeled and stems trimmed
- 2 tablespoons neutral-flavored oil like safflower or vegetable oil
- 1 ½ tablespoons white miso paste
- 1 tablespoon honey, agave or maple syrup
- 1 tablespoon rice vinegar
- 1 teaspoon reduced sodium soy sauce (or tamari)
- Optional garnish: chopped cilantro
Instructions
- Preheat the oven to 400°F.
- To make the yogurt sauce, whisk the Greek yogurt, miso paste, honey, soy sauce, and rice vinegar together in a bowl. Set aside.
- Line 2 sheet pans with parchment paper. Spread the carrots out on the sheet pans in a single layer. If any of the carrots are very large, slice them in half lengthwise.
- Whisk the oil, miso paste, honey, rice vinegar, and soy sauce together in a bowl until smooth. Reserve a small amount of the sauce to pour on the carrots after they’re done cooking. Pour the rest of the sauce on the carrots and toss to coat them evenly.
- Roast carrots in the oven 25-30 minutes until caramelized and softened, turning them halfway through. Remove the carrots from the oven and pour the remaining sauce on them. Toss to combine.
- Arrange the carrots on a serving platter and drizzle some yogurt sauce on top. Garnish with cilantro
Talk to your doctor to make sure this recipe is good for you.

Blueberry Mango Zinger Smoothie
After a C. diff infection is gone, maintaining gut health is also important. Kee Kee, a C. diff infection survivor, shared her story—and part of it was creating her own post-infection recipe.
Ingredients
- 1 cup plain kefir
- ¼ cup rolled oats
- 1 tablespoon pumpkin seeds
- 1 tablespoon chia seeds
- 1 teaspoon fresh ginger
- ¼ teaspoon ground turmeric
- Pinch of black pepper
- ½ cup frozen wild blueberries
- ½ cup frozen mango
Optional add-ins:
- 1 tablespoon nut butter for taste
- 1 cup non-dairy milk (if the smoothie is too thick)
Blend all ingredients in a blender until smooth and creamy.
Talk to your doctor to make sure this recipe is good for you.
Try this smoothie after you’ve recovered from your C. diff infection.
What about probiotics?
Probiotics are not recommended for use to prevent or treat a C. diff infection. They can be taken safely when your gut is in a healthy state, and they are designed to help maintain a healthy gut microbiome.20,21
In fact, after antibiotic treatment, probiotics may actually stop the process by which the microbiome develops a more normal balance of bacteria.22
Before taking any supplements, it is important to talk to your doctor.
C. diff Info Center
Advocacy groups
is building a nationwide C. diff awareness movement by educating the public, empowering advocates, and shaping policy. The Foundation website is a resource for information and to get involved with helping raise awareness about C. diff infections.
is the leading global patient, family, caregiver and healthcare organization educating and advocating for C. difficile infection prevention, treatments, clinical trials, diagnostics, support, and environmental safety worldwide.
More information sources
Ferring Pharmaceuticals is
committed to developing
microbiome-based therapies for
recurrent C. diff infections.
From the (CDC):
“The Progression of a C. diff
Infection” gives you quick facts
on what to expect with a C. diff
infection.
From the
(AGA): “Navigating Your C. diff
Diagnosis” is helpful reading for
patients and caregivers.
References
- Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;372(16):1539-1548.
- Gilbert JA, Blaser MJ, Caporaso JG, Jansson JK, Lynch SV, Knight R. Current understanding of the human microbiome. Nat Med. 2018;24(4):392-400.
- Antharam VC, Li EC, Ishmael A, et al. Intestinal dysbiosis and depletion of butyrogenic bacteria in Clostridium difficile infection and nosocomial diarrhea. J Clin Microbiol. 2013;51(9):2884-2892.
- Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017;474(11):1823-1836.
- Bien J, Palagani V, Bozko P. The intestinal microbiota dysbiosis and Clostridium difficile infection: is there a relationship with inflammatory bowel disease? Therap Adv Gastroenterol. 2013;6(1):53-68.
- Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825-834.
- Cornely OA, Miller MA, Louie TJ, Crook DW, Gorbach SL. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis. 2012;55(suppl 2):s154-s161.
- Smits WK, Lyras D, Lacy DB, Wilcox MH, Kuijper EJ. Clostridium difficile infection. Nat Rev Dis Primers. 2016;2(16020):1-47.
- Kelly CP. Can we identify patients at high risk of recurrent Clostridium difficile infection? Clin Microbiol Infect. 2012;18(suppl 6):21-27.
- Fernandez-Garcia L, Blasco L, Lopez M, Tomas M. Clostridium difficle infection: pathogenesis, diagnosis, and treatment, Clostridium difficile – A Comprehensive Overview, Shymaa Enany, Intech Open, doi: 10.5772/67754. Available from: https://www.intechopen.com/chapters/54496
- Guh AY, Mu Y, Winston LG, et al, for the Emerging Infections Program Clostridioides difficile Infection Working Group.Trends in U.S. burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2020;382(14):1320-1330.
- Marchesi JR, Adams DH, Fava F, et al. The gut microbiota and host health: a new clinical frontier. Gut. 2016;65(2):330-339.
- Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infection. Am J Gastroenterol. 2013;108(4):478-498.
- McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):e1-e48.
- Johnson S, Lavergne V, Skinner AM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 Focused Update Guidelines on Management of Clostridioides difficile Infection in Adults. Clin Infect Dis. 2021;73(5):e1029-e1044.
- Staley C, Khoruts A, Sadowsky MJ. Contemporary applications of fecal microbiota transplantation to treat intestinal diseases in humans. Arch Med Res. 2017;48(8):766-773.
- Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med. 2016;8(1):39.
- Tariq R, Pardi DS, Bartlett MG, Khanna S. Low cure rates in controlled trials of fecal microbiota transplantation for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Clin Infect Dis. 2019;68(8):1351-1358.
- Riddle DJ, Dubberke ER. Clostridium difficile infection in the intensive care unit. Infect Dis Clin North Am. 2009;23(3):727-743
- Cordaillat-Simmons M, Rouanet A, Pot B. Live biotherapeutic products: the importance of a defined regulatory framework. Exp Mol Med. 2020;52:1397-1406.
- Kelly CR, Fischer M, Allegretti JR, et al. ACG Clinical Guidelines: Prevention, Diagnosis, and Treatment of Clostridioides difficile Infections. Am J Gastroenterol. 2021;116:1124-1147.
- Suez J, Zmora N, Ziblerman-Schapira G, et al. Post-antibiotic gut mucosal microbiome reconstitution is impaired by probiotics and improved by autologous FMT. Cell. 2018;174(6):1406-1423.
- Rodrigues R, Barber GE, Ananthakrishnan AN. A comprehensive study of costs associated with recurrent Clostridioides difficile infection. Infect Control Hosp Epidemiol. 2017;38(2):196-202.
- Unni S, Scott T, Boules M, Teigland C, Parente A, Nelson W. Healthcare burden and costs of recurrent Clostridioides difficile infection in the Medicare population. Presented at: AMCP 2020; April 21-24, 2020; Houston, TX.
- Lurienne L, Bandinelli P, Galvain T, Coursel C, Oneto C, Feuerstadt P. Perception of quality of life in people experiencing or having experienced a Clostridioides difficile infection: a US population survey. J Patient Rep Outcomes. 2020;4(1):14.
- Mayo Clinic website. 2021 C. diff – Diagnosis and treatment https://www.mayoclinic.org/diseases-conditions/c-difficile/diagnosis-treatment/drc-20351697. Accessed September 25, 2021.
- Ward C, Kelly CR. Clostridioides difficile infection: Is there a role for diet and probiotics? Pract Gastroenterol. 2020;44(9):26-34.
You are about to leave this site.
By clicking continue, you will be directed to a site about a prescription treatment option for the prevention of recurrent C. diff infection. Would you like to continue?