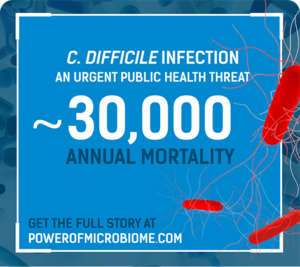
November is C. diff Awareness Month
Ferring is dedicated to helping patients with recurrent C. diff infection live better lives
Power of the Microbiome
Can It Be Unlocked to Break the
Cycle of Recurrent C. difficile Infection?
Get the full microbiome story
A diverse microbial composition is essential to overall health. Bacteroidetes and Firmicutes, the gut’s most prevalent phyla, are vital to maintaining overall health and inhibiting C. difficile infection.
Dysbiosis creates an insufficiency of Bacteroidetes and Firmicutes, which may lead to an environment suited for C. difficile growth.
Antibiotic treatment—including vancomycin and fidaxomicin—address the acute infection but do not address (and possibly worsen) dysbiosis or restore the diverse microbial composition—allowing a window of vulnerability for recurrence.
While efficacious, historic approaches to microbiome restoration—including fecal microbiota transplantation and probiotics—have disadvantages.
Patients may face significant complications including sepsis, colectomy, and mortality. The healthcare system faces significant challenges including high admission rates, lengths of stays, and care costs.
Mechanism of Disease
Microbiome Experts Videos
Hear from microbiome content experts discussing everything from disease burden to patient perspectives
Microbiome Restoration—The Limitations of Current Data
Microbiome Experts Videos
Hear from microbiome content experts discussing everything from disease burden to patient perspectives
Mechanism of CDI
EXPLORE THE MICROBIOME

RESOURCES AND TOOLS

SPEAKER PROGRAMS:
LEARN FROM THE EXPERTS
Use the menu to view the different
sections on the microsite
#ferringmicrobiome