Get the full story of the microbiome
- Importance of Microbial Diversity
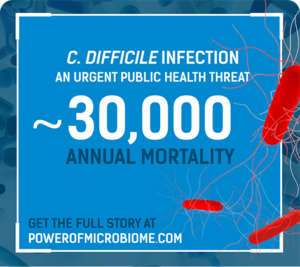
- Dysbiosis and Recurrent C. difficile Infection
- Historic Microbiome Restoration Approaches
- Patient and Healthcare Burdens
Historic approaches to microbiome restoration have limitations
The aim of microbiome restoration is to repopulate
a diverse gut microbiota to treat disease.
For recurrent C. difficile infection (rCDI), one approach is fecal microbiota transplantation (FMT). FMT has been shown to be efficacious in treating rCDI and reestablishing gut biodiversity.1 However...

Treatment
- Resource intensive: may involve bowel preparation, anesthesia, NG tubes, and risk of perforation2
- FDA has issued multiple safety alerts regarding the potential risk of serious or life-threatening infections following FMT3
-Not FDA-approved: no regulated testing criteria for safety or standardized manufacturing4,5 - Digestive environment may compromise FMT microorganisms delivered orally6,7

Clinical studies
Most data are from retrospective case series or systemic reviews with considerable variability.8
Treatment success in 13 clinical trialsa of single-dose FMT8
- This inconsistency is due to considerable heterogeneity among randomized controlled trials, with marked differences in study structure, control groups, fecal transplant materials, and outcome assessments9,10
- Patients enrolled in clinical trials may not be a true reflection of patients seen in the real world. Strict inclusion and exclusion criteria in randomized controlled trials lead to inclusion of a small portion of patients from daily clinical practice, limiting generalizability of results to patients seen in clinical practice8
Probiotics do not restore the microbiome nor address dysbiosis
- Designed to help maintain a healthy gut microbiome11
- Clinical guidelines recommend against probiotics for the prevention of rCDI12
- May hinder normal colon recolonization following antibiotic treatment13
A safe, regulated, and reliable option is vitally needed to reduce
the burdens of CDI and recurrence.
FDA, US Food and Drug Administration; NG, nasogastric.
aMeta-analysis.
THE BURDEN OF CDI MAY INCREASE
WHEN THE INFECTION RECURS
Can the power of the microbiome be
unlocked to break the cycle of rCDI?
Share this with colleagues!
References
- Van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407-415.
- Allegretti JR, Korzenik JR, Hamilton MJ. Fecal microbiota transplantation via colonoscopy for recurrent C. difficile infection. J Vis Exp. 2014;(94):52154.
- US Food and Drug Administration website. Fecal Microbiota for Transplantation: Safety Alert–Risk of Serious Adverse Events Likely Due to Transmission of Pathogenic Organisms. https://www.fda.gov/safety/medical-product-safety-information/fecal-microbiota-transplantation-safety-alert-risk-serious-adverse-events-likely-due-transmission. Accessed March 12, 2022.
- US Food and Drug Administration website. Early Clinical Trials with Live Biotherapeutic Products: Chemistry, Manufacturing, and Control Information: Guidance for Industry. https://www.fda.gov/files/vaccines,%20blood%20&%20biologics/published/Early-Clinical-Trials-With-Live-Biotherapeutic-Products–Chemistry–Manufacturing–and-Control-Information–Guidance-for-Industry.pdf. Accessed March 12, 2022.
- McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):e1-e48.
- Hirsch BE, Saraiya N, Poeth K, Schwartz RM, Epstein ME, Honig G. Effectiveness of fecal-derived microbiota transfer using orally administered capsules for recurrent Clostridium difficile infection. BMC Infect Dis. 2015;15:191.
- Kao D, Roach B, Silva M, et al. Effect of oral capsule–vs colonoscopy-delivered fecal microbiota transplantation on recurrent Clostridium difficile infection. JAMA. 2017;318(20):1985-1993.
- Tariq R, Pardi DS, Bartlett MG, Khanna S. Low cure rates in controlled trials of fecal microbiota transplantation for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Clin Infect Dis. 2019;68(8):1351-1358.
- Bafeta A, Yavchitz A, Riveros C, Batista R, Ravaud P. Methods and reporting studies assessing fecal microbiota transplantation: a systematic review. Ann Intern Med. 2017;167(1):34-39.
- Feuerstadt P, Aroniadis OC, Svedlund FL, et al. Heterogeneity of randomized controlled trials of fecal microbiota transplantation in recurrent Clostridiodes difficile infection. Dig Dis Sci. 2022;67(7):2763-2770.
- Cordaillat-Simmons M, Rouanet A, Pot B. Live biotherapeutic products: the importance of a defined regulatory framework. Exp Mol Med. 2020;52(9):1397-1406.
- Kelly CR, Fischer M, Allegretti JR, et al. ACG Clinical Guidelines: prevention, diagnosis, and treatment of Clostridioides difficile infections. Am J Gastroenterol. 2021;116(6):1124-1147.
- Suez J, Zmora N, Ziblerman-Schapira G, et al. Post-antibiotic gut mucosal microbiome reconstitution is impaired by probiotics and improved by autologous FMT. Cell. 2018;174(6):1406-1423.e16.
